Prolia is a medication used to treat osteoporosis, but is it worth the risk? According to the FDA, Prolia is a biologic medication that has been shown to increase bone density and reduce the risk of vertebral fractures in postmenopausal women with osteoporosis.
The risk of Prolia includes a higher risk of serious infections, such as pneumonia, and also an increased risk of bone, joint, or muscle pain.
Prolia has also been linked to a condition called osteonecrosis of the jaw, which can be painful and may require surgery to treat.
What is Prolia?
Prolia, also known as denosumab, is a medication that helps make your bones stronger and reduces the risk of broken bones.
It works by blocking the formation and activity of cells that break down bone, restoring the balance and making your bones stronger.
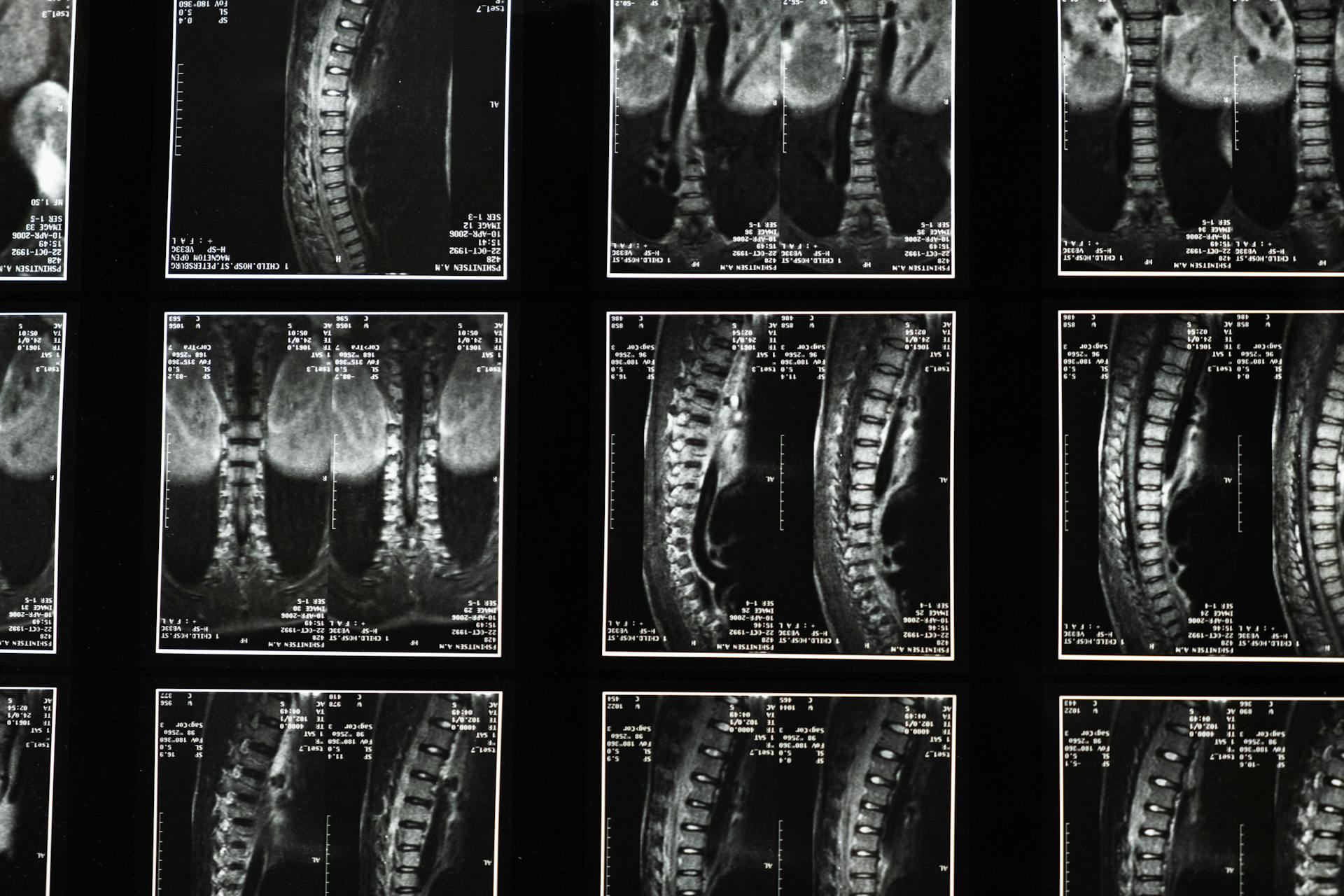
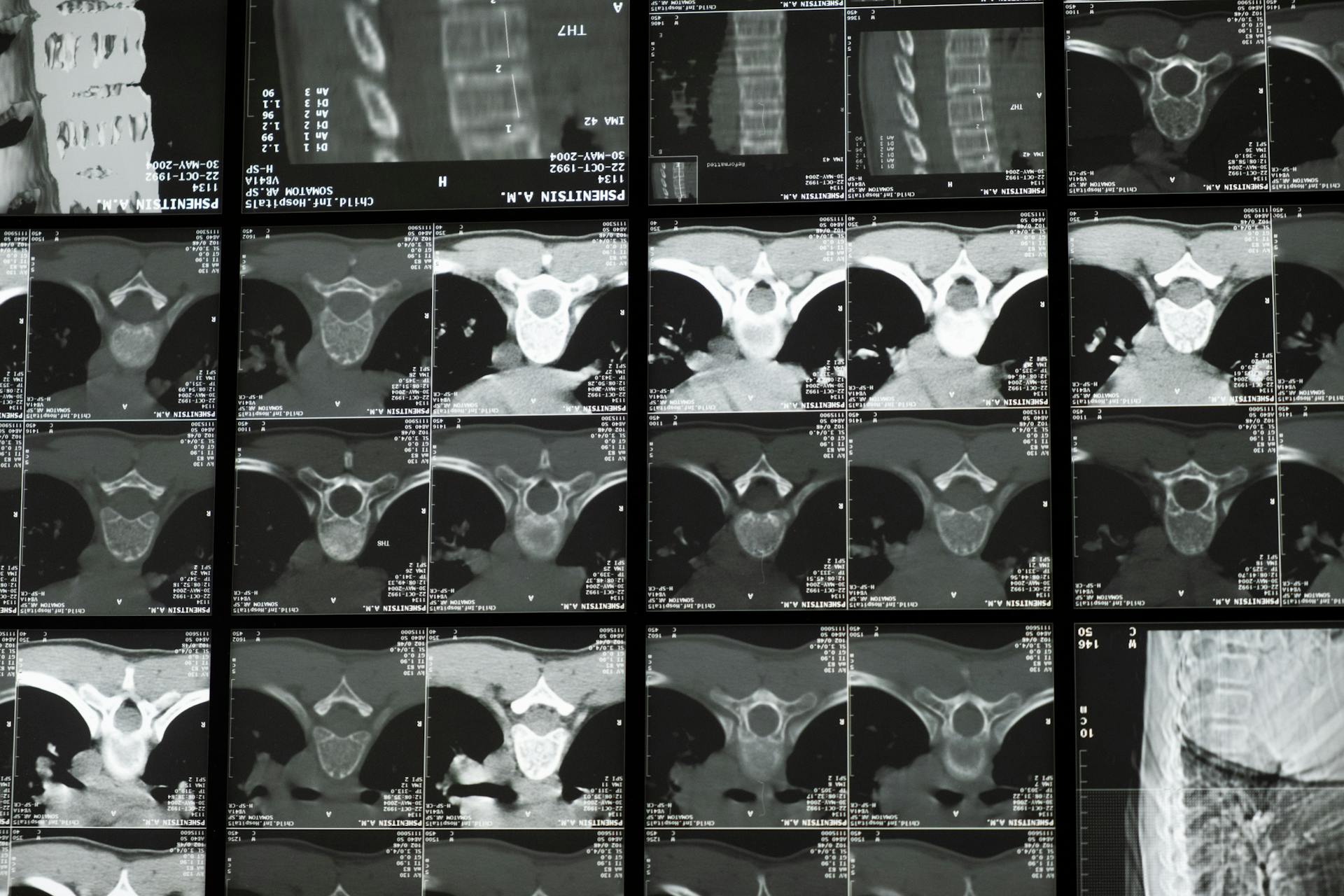
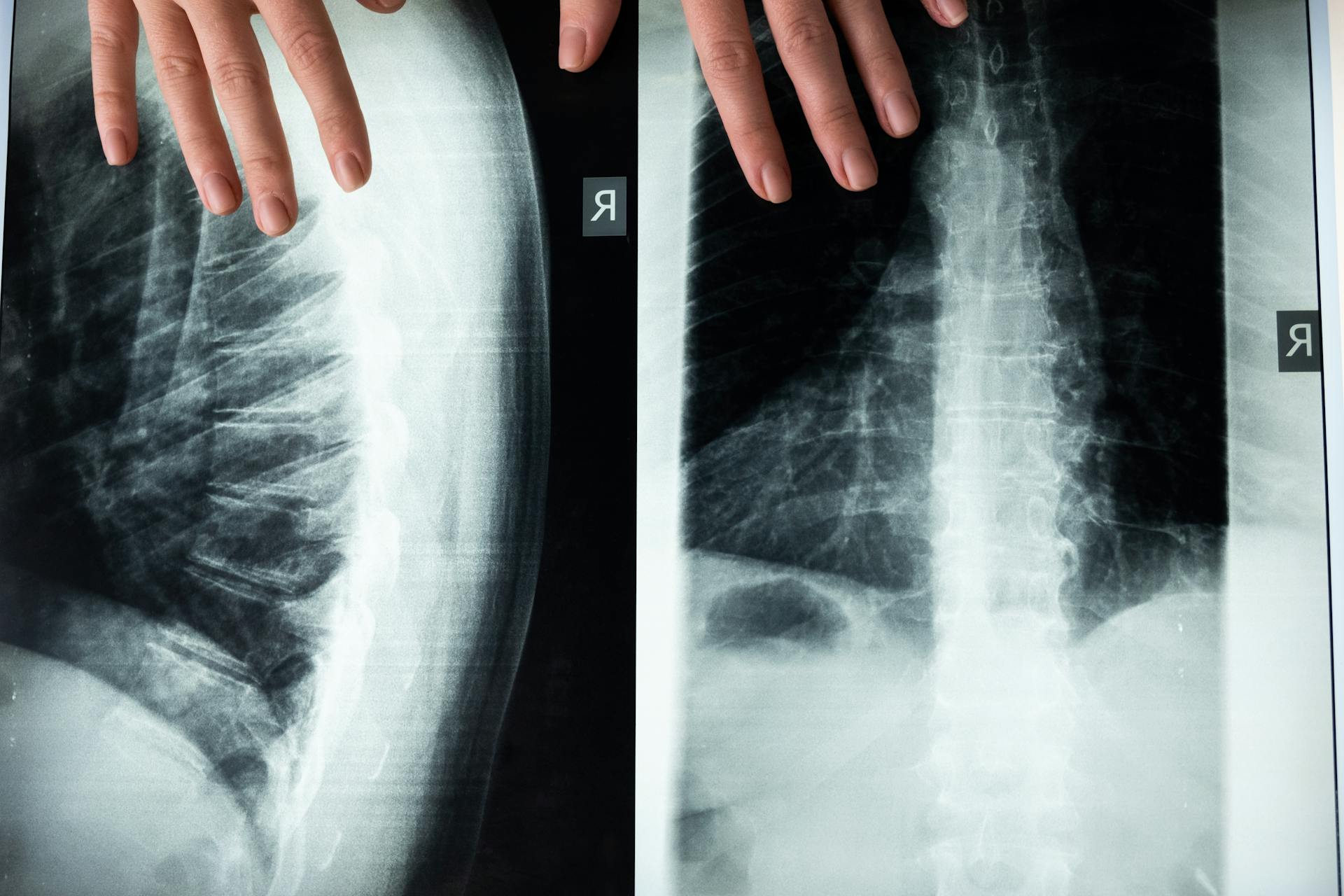
Bones are made up of living tissue and are constantly being broken down and rebuilt by specialist bone cells.
Taking denosumab will make fractures much less likely, but it's still possible to break a bone even while taking the medication.
Denosumab is not a pain-relieving medicine, so it won't reduce the pain caused by broken bones.
Eligibility and Suitability
Denosumab, the medication also known as Prolia, is typically offered to people with osteoporosis or a high risk of breaking a bone. You might be a good candidate if you've already tried a different treatment for your bones.
Denosumab is licensed for use in women who have been through the menopause, as well as men.
Eligibility for Denosumab
You're considering denosumab as a treatment option, but first, let's talk about who can have it. Denosumab may be suitable for you if you have osteoporosis or a high risk of breaking a bone.
Denosumab can be used as a first treatment, but it's usually only an option if you've tried a different drug treatment for your bones or if other drugs aren't suitable for you. This is because denosumab works best when used after other treatments have been tried.
Denosumab is licensed for use in women who have been through the menopause and for men. Your doctor may occasionally offer it to younger women, but this is less common.
To be eligible for denosumab, you'll need to have a high risk of breaking a bone or osteoporosis. Your doctor will assess your individual situation to determine if denosumab is the right treatment for you.
Not Suitable For

If you're considering taking denosumab, there are certain situations where it's not suitable.
If you have a low blood calcium level, you'll need to increase your intake of calcium and vitamin D before you can start denosumab.
Having an intolerance to sorbitol, a type of sugar, is another reason denosumab may not be suitable for you.
Pregnant or breast-feeding women should also avoid taking denosumab.
Here are some specific conditions where denosumab is not recommended:
- Low blood calcium level (hypocalcaemia)
- Intolerance to sorbitol
- Pregnancy or breast-feeding
Treatment and Monitoring
You'll have regular appointments to receive your injection, typically every six months, and you should contact your healthcare professional if you have any issues in between.
A blood test is usually required before each injection to check your calcium levels, kidney function, and sometimes vitamin D levels. Some people may also have a blood test two weeks after each injection.
You'll have a formal treatment review after about five years on denosumab to check if it's still the right treatment for you. Your doctor will consider whether you've broken any bones since starting treatment and may order a bone density scan.
Intriguing read: Risk Levels
If you do break a bone while taking denosumab, it doesn't necessarily mean your treatment isn't working. You should speak to your GP and consider a bone health assessment.
Here are some possible next steps after your treatment review:
- Stay on denosumab for another five years
- Change to a different drug treatment, usually a bisphosphonate
- See a specialist if you want to stop denosumab and need advice on what to do next
Monitoring My Treatment
Monitoring My Treatment is an essential part of staying healthy while on denosumab.
You'll need to have an appointment every six months to receive your injection. Your healthcare professional will check on you and make sure everything is going smoothly.
If you have any problems in between appointments, don't hesitate to reach out to your healthcare professional. They can offer advice and support to help manage any side effects.
Before each injection, you'll likely need to have a blood test. This will check your calcium levels, how well your kidneys are working, and sometimes your vitamin D levels. Some people will also have a blood test two weeks after each injection.
Breaking a bone while taking denosumab doesn't necessarily mean your treatment isn't working. However, it's a good idea to speak to your GP and possibly have a bone health assessment.
After about five years on denosumab, you'll have a formal treatment review. Your doctor will check if denosumab is still the right treatment for you.
Here are some possible next steps after your treatment review:
- stay on denosumab for another five years
- change to a different drug treatment – usually a type of drug called a bisphosphonate
- see a specialist if you want to stop denosumab and need advice on what to do next.
Denosumab Treatment Duration
You can stay on denosumab for several years before moving to a different drug treatment, but your doctor will advise you on what's best for your situation.
There is no formal guidance on how long you should be on denosumab, which means it's up to your doctor to decide.
You'll need to plan ahead with your doctor to ensure you don't experience the 'rebound effect', where you're at risk of several spinal fractures after stopping treatment.
This 'rebound effect' can happen within months of stopping denosumab, which is why it's essential to have an arrangement with your doctor to get another treatment on time.
You may not need to take another treatment if you've been on denosumab for less than two years, but it's best to discuss this with a specialist.
Denosumab wears off quickly, which means you can't stop having it for a while, unlike some other treatments that keep working for a while after you stop taking them.
Risks and Side Effects
Taking Prolia comes with a range of potential side effects, some of which can be serious. For example, severe skin infections are a rare but possible outcome, affecting less than 1 in 100 people.
Common side effects include back pain, arm and leg aches, elevated cholesterol, and general musculoskeletal pain. These issues can be managed with the help of your doctor.
Prolia can also lead to low blood calcium levels, which can cause numbness or tingling in your fingers, toes, or around your mouth. Regular blood tests can help monitor this.
If you do experience side effects, it's essential to talk to your doctor immediately. They can help you determine the cause and find ways to manage the problem.
Here are some of the possible side effects of Prolia, along with their frequency:
Some people may experience severe hypocalcemia, which can lead to heart rhythm irregularities, confusion, seizures, face twitching, and muscle spasms or weakness. This is a serious condition that requires immediate medical attention.
Watch Out for Double-Speak
Prolia and bisphosphonates may seem like effective solutions for osteoporosis, but they can have some serious side effects. Both drugs alter normal bone metabolism, which can lead to potential long-term consequences.
Sudden femoral fractures are linked to long-term bisphosphonate therapy, which can be attributed to the lack of bone remodeling. This is a warning sign that something is not quite right with these treatments.
The risks associated with Prolia and bisphosphonates include low calcium levels, serious skin and bladder infections, and severe jaw bone problems like osteonecrosis of the jaw. These side effects are no joke.
Additional reading: How Long after I Take Diflucan Can I Take Xanax?
Here are some of the potential risks associated with Prolia and bisphosphonates:
- Low calcium levels
- Serious skin, lower abdomen, bladder, or ear infections
- Dermatitis, rash, or eczema
- Inflammation of the inner lining of the heart (endocarditis) caused by an infection
- Severe jaw bone problems such as osteonecrosis of the jaw.
Denosumab, the active ingredient in Prolia, works by blocking the formation and activity of cells that break down bone. This may sound like a good thing, but it's essential to weigh the risks and benefits before making a decision.
The truth is, no medication can completely prevent fractures, and taking denosumab doesn't guarantee that you won't break a bone. However, it can make fractures much less likely.
Denosumab Side Effects
Denosumab can cause a range of side effects, but most people don't experience any problems. The most common side effects are severe skin infections, low blood calcium levels, atypical thigh bone fractures, and osteonecrosis of the jaw, all of which are rare.
Severe skin infections are a rare but serious side effect, affecting less than 1 in 100 people. If you experience any redness, swelling, or soreness of the skin, talk to your doctor immediately.
Low blood calcium levels are another rare side effect, affecting less than 1 in 1,000 people. You'll need regular blood tests to check your calcium levels, and tell your doctor if you experience numbness or tingling in your fingers, toes, or around your mouth, or muscle stiffness, spasms, twitches, or cramps.
Atypical thigh bone fractures are a rare side effect, affecting less than 1 in 1,000 people. If you experience unexplained pain in your thigh, groin, or hip that doesn't go away, talk to your doctor.
Osteonecrosis of the jaw is a rare side effect, affecting less than 1 in 1,000 people. To minimize this risk, maintain good oral hygiene and have regular dental check-ups.
If you experience any side effects that don't go away, it may help to:
- Make sure the problem isn't caused by any other medication you're taking
- Tell your doctor or pharmacist, who may be able to help find out what's causing the problem
- Ask your doctor or pharmacist about other treatments that may suit you better
Here's a summary of the most common side effects of denosumab:
Frequently Asked Questions
Why do doctors push Prolia?
Doctors recommend Prolia because it effectively stops bone-removing cells, reducing the risk of fractures in postmenopausal women with osteoporosis. This convenient, 6-month injection helps protect bones and prevent painful fractures.
What is the success rate of Prolia?
Prolia reduces the risk of new spine fractures by 68% in women, with only 2.3% experiencing new fractures compared to 7.2% in those not treated with Prolia. This significant reduction in fracture risk makes Prolia a highly effective treatment option.
Sources
- https://www.uclahealth.org/news/article/ask-the-doctors-should-i-take-a-bone-building-drug-for-osteoporosis
- https://theros.org.uk/information-and-support/osteoporosis/treatment/denosumab/
- https://www.everydayhealth.com/osteoporosis/fda-issues-warning-on-serious-risks-from-common-osteoporosis-drug/
- https://www.inspire.com/groups/bone-health-and-osteoporosis/discussion/to-take-prolia-or-take-risk-of-fracture/
- https://saveourbones.com/prolia-denosumab-review/
Featured Images: pexels.com